Written By: Shreya Bendsure, BPharm
Reviewed By: Ayurvedacharya Dr. Gaurav Pathare, BAMS,
Vikas Londhe MPharm
Cannabis is one of the oldest cultivated plants and has been used for medicinal, cultural, and industrial purposes across several ancient civilizations. Historical records from China, India, the Middle East, and Greece describe its therapeutic effects as well as its psychoactive properties. Over time, the plant came to be known by names like cannabis, hemp, and marijuana. The term “marijuana” gained popularity in the early 20th century, particularly in legal and social contexts, but scientific and regulatory bodies now prefer the broader and more accurate term “cannabis.”
Historical Context and Modern Divide
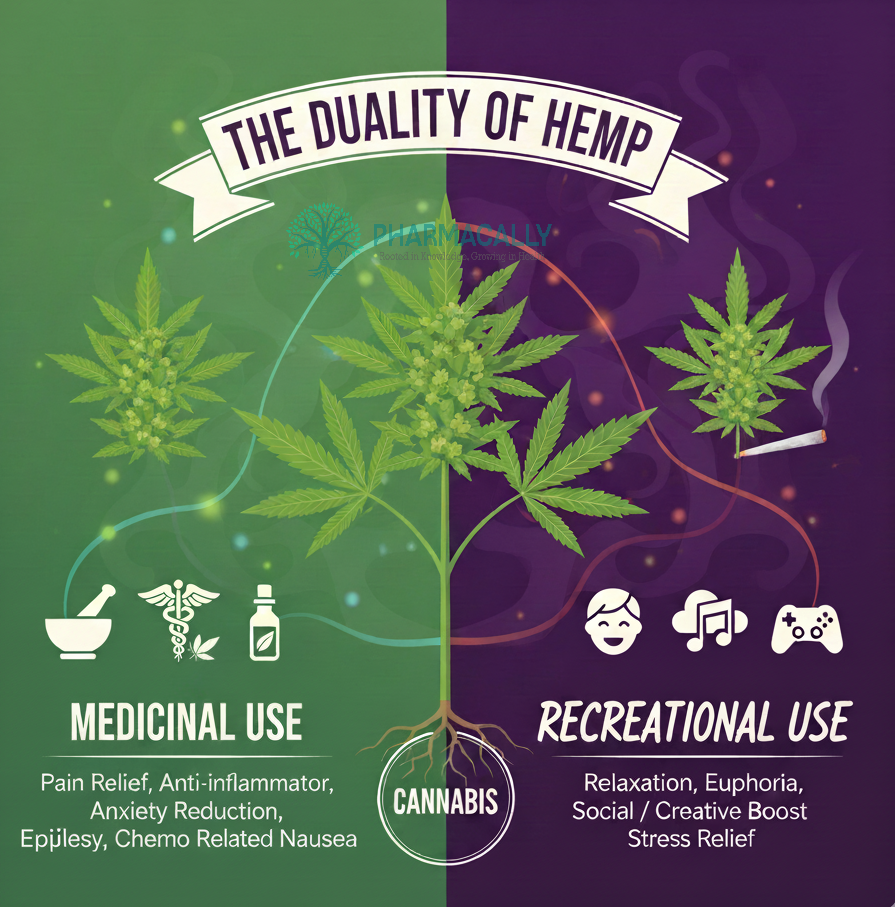
For thousands of years, cultures in China, India and Greece used cannabis for pain relief and rituals. Over time, the plant developed into two main types: hemp, which is grown for fiber and seeds, and high-resin varieties used for their cannabinoids. Today, the main difference is based on purpose. Medical cannabis is used to manage health conditions under professional guidance, while recreational cannabis is used for its psychoactive effects.
Cannabis: Medical vs Recreational Use Explained
Cannabis, one of humanity’s oldest cultivated plants, has evolved from ancient medicinal remedies to modern therapeutic and recreational products, with over 500 identified compounds driving its diverse effects.
Chemical Constituents
Cannabis potency comes from its complex mix of natural chemicals. Cannabinoids drive most of the effects, terpenes shape the aroma and influence mood, and flavonoids add antioxidant activity. This combination explains why different strains can feel so different.
Cannabinoids (100+ types): Work with the body’s endocannabinoid system, affecting pain, mood and inflammation.
Terpenes: Aromatic oils that create each strain’s scent and may contribute to calming, energizing or focusing effects.
Flavonoids: Plant pigments that provide color and may offer anti-inflammatory benefits based on early research
Compound Class | Role in Effects | Examples |
Cannabinoids | Primary therapeutic/psychoactive | THC (euphoria), CBD (calming) |
Terpenes | Mood/aroma enhancers | Myrcene (sedative), Limonene (uplifting) |
Flavonoids | Antioxidant support | Cannflavins (neuroprotective) |
THC vs CBD: The Power Duo
THC and CBD are the most studied cannabinoids, each playing a different role. THC creates the high by binding to CB1 receptors in the brain and is often used recreationally for stronger effects. CBD provides a calming influence without intoxication, making it suitable for daytime medical use. Medical products usually aim for balanced THC-CBD ratios for safety and symptom control, while recreational products often favor high THC levels for a more intense experience.
Property | THC | CBD |
Psycho-activity | High (alters perception, euphoria) | None |
Key Medical Uses | Nausea control, pain relief, appetite boost | Epilepsy (Epidiolex), anxiety reduction |
Common Risks | Paranoia, dependence at high doses | Rare, generally safe |
Binding Style | Strong CB1 receptor affinity | Indirect, multi-receptor |
Production Quality and Safety Standards
Medical cannabis is tested to pharmaceutical standards for potency, contaminants and consistency, which helps ensure safe and reliable dosing for patients. Recreational cannabis, however, is regulated differently depending on the region, leading to wide variation in quality and strength. This difference can influence dosing accuracy, safety and the overall risk of adverse effects.
Approved therapies highlight medical rigor:
Epidiolex (CBD): This purified CBD medicine is approved by the FDA and EMA for treating rare childhood epilepsies such as Dravet syndrome and Lennox-Gastaut syndrome. It represents the strongest clinical evidence for CBD in a medical setting.
Dronabinol and Nabilone: These synthetic forms of THC are approved in several countries to help manage chemotherapy-related nausea and vomiting. They provide controlled dosing and standardized formulations that are not available in most recreational products.
Sativex (THC:CBD spray): This balanced THC-CBD oral spray is approved in Europe, the United Kingdom, Canada and Australia for relieving muscle spasticity in multiple sclerosis. Its fixed ratio and metered delivery support consistent therapeutic effects.
Feature | Medical Cannabis | Recreational Cannabis |
Testing | Strictly follows GMP, tested for pesticides, metals, microbes | It varies and often minimal or no testing |
Forms | Standardized oils, capsules | Edibles, vapes, potent extracts |
Regulation | Physician oversight | State/country consumer models |
Benefits, Risks, and Smart Use
Medical cannabis has strong evidence for helping with chemotherapy-related nausea, certain childhood epilepsies and muscle spasticity in multiple sclerosis. It can also help some people with chronic pain, but the results vary. Early research suggests possible benefits for anxiety and insomnia, though the evidence is still limited. Because cannabis can affect the heart, mood and drug metabolism, medical use should be monitored by a clinician, especially when THC levels are high. These risks are even greater in recreational settings where products often contain very strong THC.
How Strong is Evidence
Strong evidence: Chemotherapy-related nausea; severe childhood epilepsy.
Moderate evidence: Chronic pain; MS-related spasticity.
Emerging or limited evidence: Anxiety; insomnia.
Risks to keep in mind
THC-related risks: Anxiety, rapid heart rate and potential for dependence.
General risks: Avoid during pregnancy and adolescence, and be cautious about interactions with other medications.
In summary, Medical and recreational cannabis differ in purpose, regulation, quality, and safety. Medical cannabis is standardized, clinically guided, and intended for treating specific symptoms under professional supervision. Recreational cannabis is used for psychoactive effects and is regulated as a consumer product rather than a medicine. Understanding these distinctions helps doctors, patients, and the general public makes informed decisions based on scientific evidence and awareness of potential risks.
References
Cannabis (Marijuana), National Institute of Drug Abuse, https://nida.nih.gov/research-topics/cannabis-marijuana
Gabarin, A et al, Cannabis as a Source of Approved Drugs: A New Look at an Old Problem. Molecules, 2023, 28, 7686. https://doi.org/10.3390/molecules28237686
Fatima-Zahrae Laaboudi et al, In the weeds: A comprehensive review of cannabis; its chemical complexity, biosynthesis, and healing abilities, Toxicology Reports, Volume 13, 2024, 101685, https://doi.org/10.1016/j.toxrep.2024.101685
Matheson J and Le Foll B (2020) Cannabis Legalization and Acute Harm From High Potency Cannabis Products: A Narrative Review and Recommendations for Public Health. Front. Psychiatry 11:591979. Doi: 10.3389/fpsyt.2020.591979
Hoch, E et al, Cannabis, cannabinoids and health: a review of evidence on risks and medical benefits. Eur Arch Psychiatry Clin Neurosci 275, 281–292 (2025). https://doi.org/10.1007/s00406-024-01880-2
Stella N. THC and CBD: Similarities and differences between siblings. Neuron. 2023 Feb 1; 111(3):302-327. Doi: 10.1016/j.neuron.2022.12.022. Epub 2023 Jan 12. PMID: 36638804; PMCID: PMC9898277.
FDA Regulation of Cannabis and Cannabis-Derived Products, Including Cannabidiol (CBD), 16 July 2025, https://www.fda.gov/news-events/public-health-focus/fda-regulation-cannabis-and-cannabis-derived-products-including-cannabidiol-cbd
Jardim, C et al, The Regulatory Environment Surrounding Cannabis Medicines in the EU, the USA, and Australia, Pharmaceutics 2025, 17, 635. https://doi.org/10.3390/pharmaceutics17050635