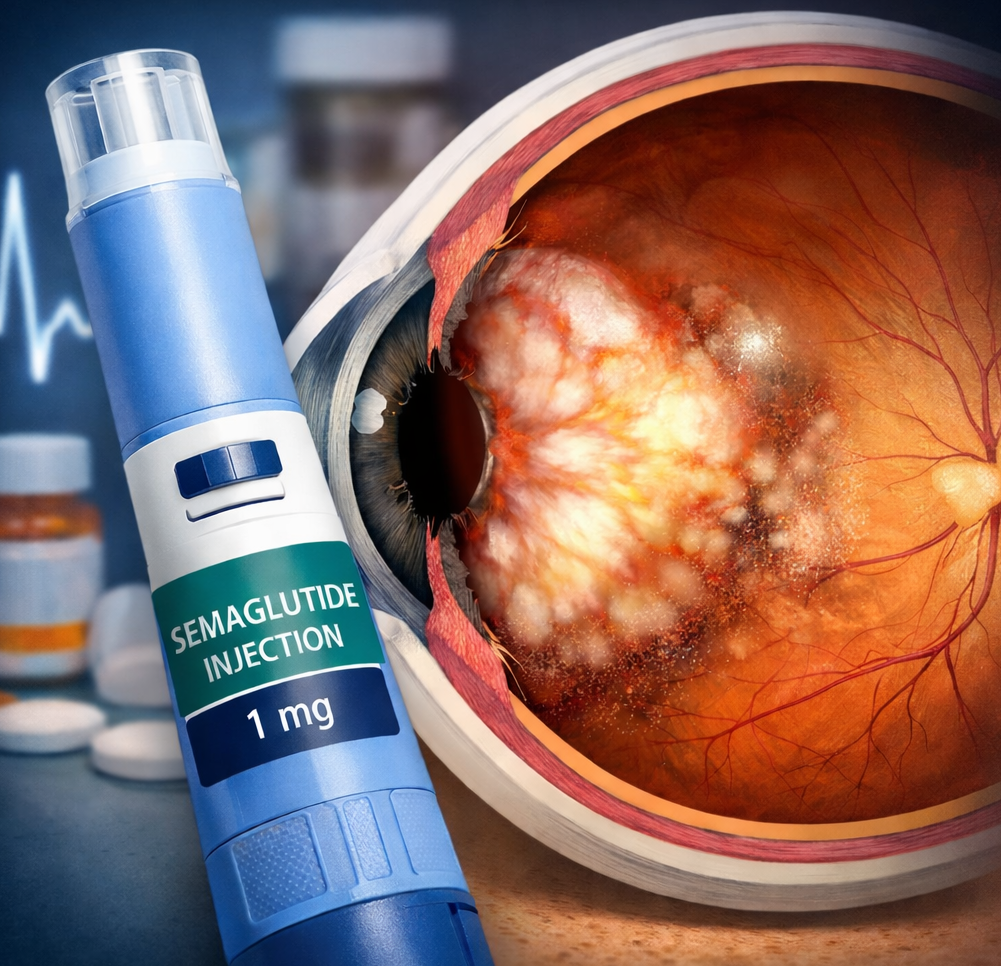
Semaglutide has been linked to rare cases of non-arteritic anterior ischemic optic neuropathy (NAION). Learn what current studies, regulators, and clinicians say about the possible risk and how to interpret it.
Written By: Abhinay Wadekar, Shreya Bendsure
and Sheetal Barbade, BPharm
Medically Reviewed By: Dr. Htet Wai Moe,
MBBS, MD, PhD-Pharmacology
Non-arteritic anterior ischemic optic neuropathy (NAION) is a rare but serious condition caused by reduced blood flow to the optic nerve. It typically presents as sudden, painless vision loss and may be permanent. The estimated annual incidence is about 2–10 cases per 100,000 people over age 50. NAION is distinct from diabetic retinopathy, which involves retinal microvascular damage and progressive changes. Instead, NAION is an acute ischemic event of the optic nerve, usually unilateral, and is more common in older adults and individuals with vascular risk factors such as diabetes, hypertension, and sleep apnea.
Recently, observational data have raised questions about a possible association between semaglutide, a GLP-1 receptor agonist used for diabetes and weight management, and NAION. The key challenge is determining whether this represents a true drug-related risk or reflects confounding factors among patients who are more likely to receive semaglutide.
Evidence from Observational Studies
A matched cohort study published in JAMA Ophthalmology reported a higher incidence of NAION in patients prescribed semaglutide compared with those receiving non-GLP-1 agents. The hazard ratio was elevated, and cumulative incidence over 36 months was higher in the semaglutide group. Subsequent and larger datasets suggest the relative risk may be smaller than this early estimate, especially when compared against agents such as empagliflozin or sitagliptin. However, these studies remain observational and cannot prove causality. Residual confounding, including differences in disease severity, may influence results.
Other cohort analyses have shown similar patterns, generally indicating a modestly higher risk of NAION among semaglutide users. A Danish population-based study involving more than 424,000 individuals with type 2 diabetes suggested that once-weekly semaglutide was associated with approximately double the five-year risk of NAION compared with other diabetes therapies. Despite this signal, the absolute number of events remained low because NAION is rare.
Case reports and small case series have described NAION occurring in patients treated with semaglutide. These reports support biological plausibility but do not establish incidence or causation. Proposed mechanisms remain hypothetical and include altered optic nerve perfusion, nocturnal hypotension related to weight loss, or individual susceptibility. At the same time, GLP-1’s anti-inflammatory effects argue against a simple pro-ischemic mechanism.
Contrasting Evidence and Key Limitations
Not all analyses demonstrate a clear increased risk. Low event numbers, short follow-up, and heterogenicity in how NAION is defined may contribute to inconsistent findings. Some systematic reviews and meta-analyses have not identified a statistically significant increase in eye disorders overall with semaglutide, and conclusions specific to NAION remain uncertain because of limited data.
Across nearly all studies, confounding by indication is a central limitation. People prescribed semaglutide often have more advanced diabetes, higher body mass index, or additional vascular risk factors that independently increase the likelihood of NAION. Although statistical adjustments are used, unmeasured or residual bias cannot be excluded.
Regulatory Reviews and Safety Communications
As observational evidence accumulated, regulators evaluated the potential safety signal. In June 2025, the World Health Organization issued a medical product alert highlighting NAION as a potential risk associated with semaglutide-containing medicines (Ozempic, Wegovy, and Rybelsus). WHO recommended that risk management plans be updated and that additional pharmacovigilance activities be implemented. The alert does not confirm causation; instead, it recognizes a signal that warrants monitoring.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee similarly reviewed post-marketing data. NAION is now listed as a very rare adverse effect in product information. This classification reflects a regulatory risk signal category, not a precise measurement of true incidence in all users. Current determinations apply specifically to semaglutide products and are not automatically extended to the entire GLP-1 class.
How to Interpret the Evidence Clinically
Even with consistent observational associations, several points remain critical:
- Confounding remains likely. Semaglutide users often carry higher baseline vascular risk. Adjustments reduce but may not eliminate bias.
- Absolute risk is low. NAION is rare, and the number of events remains small relative to widespread semaglutide use.
- Causality is unproven. Randomized clinical trials have not confirmed a direct causal link, and most were not designed or powered to detect such rare events.
- Mechanisms are speculative. No definitive biological pathway has been demonstrated.
Practical Guidance for Clinicians and Patients
Current evidence suggests an association between semaglutide and NAION, but not definitive proof of causation. Benefits of semaglutide in glycemic control, weight reduction, and cardiovascular risk mitigation remain well established. Decisions should therefore be individualized rather than reflexively discontinuing therapy.
Clinicians should:
- Discuss the possibility of very rare ocular events during shared decision-making.
- Advise patients to report sudden, painless vision loss or new visual field defects immediately.
- Consider prompt ophthalmologic referral if symptoms appear.
- Exercise added caution in individuals with prior NAION, crowded optic discs, severe untreated sleep apnea, or poorly controlled vascular risk factors.
- Reassess treatment only after clinical evaluation instead of stopping semaglutide routinely.
Key Points for Practice
- Extra vigilance is reasonable in patients with prior NAION or high optic nerve vulnerability.
- Educate patients on symptoms that require urgent evaluation.
- Continue semaglutide when benefits outweigh risks, using case-by-case judgment.
- Support ongoing pharmacovigilance and research to clarify causality and identify higher-risk subgroups.
The potential link between semaglutide and NAION has emerged through observational research and subsequent regulatory review. While the absolute risk appears very low, NAION’s potential for irreversible vision loss justifies careful monitoring and informed counselling. At present, the evidence supports vigilance, not blanket avoidance, while further studies work to determine whether the association reflects true causality or confounding.
References
Hathaway JT, Shah MP, Hathaway DB, et al. Risk of Nonarteritic Anterior Ischemic Optic Neuropathy in Patients Prescribed Semaglutide. JAMA Ophthalmol. 2024;142(8):732–739. doi:10.1001/jamaophthalmol.2024.2296
Cai CX, Hribar M, Baxter S, et al. Semaglutide and Nonarteritic Anterior Ischemic Optic Neuropathy. JAMA Ophthalmol. 2025;143(4):304–314. doi:10.1001/jamaophthalmol.2024.6555
Grauslund, J., Taha, A.A., Molander, L.D. et al. Once-weekly semaglutide doubles the five-year risk of nonarteritic anterior ischemic optic neuropathy in a Danish cohort of 424,152 persons with type 2 diabetes. Int J Retin Vitr 10, 97 (2024). https://doi.org/10.1186/s40942-024-00620-x
Ahmadi H, Hamann S. Anterior ischemic optic neuropathy in patients treated with semaglutide: report of four cases with a possible association. BMC Ophthalmol. 2025 Mar 14;25(1):132. Doi: 10.1186/s12886-025-03958-4. PMID: 40087651; PMCID: PMC11908077.
Lešin Gaćina, D., Vidović, T., Vlajić Oreb, N., Matković, L., & Jandroković, S. (2025). Is Semaglutide Linked to NAION? A Case Report on a Rare Ocular Complication. Reports, 8(3), 149. https://doi.org/10.3390/reports8030149
Natividade GR et al, Ocular Adverse Events with Semaglutide: A Systematic Review and Meta-Analysis. JAMA Ophthalmol. 2025 Sep 1;143(9):759-768. doi: 10.1001/jamaophthalmol.2025.2489. PMID: 40810985; PMCID: PMC12355393.
Semaglutide Not Associated with Increased Risk of Eye Disorders, 19 August 2025, https://www.ajmc.com/view/semaglutide-not-associated-with-increased-risk-of-eye-disorders
The use of semaglutide medicines and risk of non-arteritic anterior ischemic optic neuropathy (NAION), 27 June 2025, WHO, https://www.who.int/news/item/27-06-2025-27-06-2025-semaglutide-medicines-naion
PRAC concludes eye condition NAION is a very rare side effect of semaglutide medicines Ozempic, Rybelsus and Wegovy, 06 June 2025, European Medicine Agency, https://www.ema.europa.eu/en/news/prac-concludes-eye-condition-naion-very-rare-side-effect-semaglutide-medicines-ozempic-rybelsus-wegovy
Kai-Yang Chen, Hoi-Chun Chan, Chi-Ming Chan, does semaglutide increase the risk of non-arteritic anterior ischemic optic neuropathy? A systematic review and meta-analysis of emerging evidence, Asia-Pacific Journal of Ophthalmology, 2025, 100245, https://doi.org/10.1016/j.apjo.2025.100245