Abbott presented new five-year data at NANS 2026 showing its spinal cord stimulation and dorsal root ganglion neuromodulation therapies reduced pain-related healthcare visits by up to 75% and expanded MRI access for chronic pain patients.
Written By: Pharmacally Medical News Desk
Abbott has announced new five-year clinical data showing that its neuromodulation therapies can significantly reduce pain-related healthcare visits for people living with chronic pain. The findings were presented at the North American Neuromodulation Society (NANS) 2026 Annual Meeting in Las Vegas and highlight the long-term benefits of Abbott’s proprietary technologies, including BurstDR™ spinal cord stimulation (SCS) and dorsal root ganglion (DRG) stimulation.
Chronic pain affects more than one in five people in the United States and is associated with an economic burden of nearly $723 billion annually, driven by medical expenses and productivity loss. Patients living with chronic pain often require frequent office visits, repeat imaging, ongoing medications, and physical therapy, making the condition both costly and disruptive to daily life.
Long-Term Evidence Shows Reduced Healthcare Utilization
A retrospective analysis presented at NANS found that Abbott’s spinal cord stimulation therapy led to a major decline in pain-related healthcare use. Patients using Abbott’s SCS system reduced their pain-related medical visits by an average of 75% after five years.
According to Timothy Deer, M.D., lead author of the study, spinal cord stimulation can dramatically lessen the burden placed on patients by reducing the need for repeated medical interventions and helping individuals regain normal function.
Additional real-world evidence came from a separate study involving 834 patients implanted with Abbott’s Proclaim™ DRG system for chronic pain conditions such as complex regional pain syndrome (CRPS), peripheral neuropathy, failed back surgery syndrome, and chronic back pain. At five years, these patients experienced an average 73% reduction in pain-related healthcare use, supporting the durability of Abbott’s DRG stimulation approach across multiple pain indications.
Strong Patient Preference for BurstDR Stimulation
Abbott also reported sustained long-term patient satisfaction with its BurstDR™ waveform technology. In a five-year study of 127 patients, 92% reported a preference for BurstDR stimulation over traditional tonic stimulation, which is often associated with tingling sensations. BurstDR delivers mild bursts of electrical pulses designed to alter pain signaling between the spinal cord and the brain.
Patients implanted with Abbott’s SCS systems also demonstrated continued improvements in physical function and pain relief over more than five years, researchers observed reductions in pain catastrophizing, with patient-reported outcomes approaching levels seen in healthy populations.
FDA Approval Expands MRI Access for Abbott Neuromodulation Patients
Alongside the clinical updates, Abbott announced it has received FDA approval for prone MRI scanning with its chronic pain neuromodulation portfolio. The expanded MRI labeling applies to both new and existing patients implanted with Abbott systems, including the Proclaim™ SCS family, the Eterna™ SCS system, and the Proclaim™ DRG neurostimulation system.
Prone MRI compatibility is especially important for diagnostic evaluations that require face-down positioning, such as breast cancer imaging and certain upper-extremity scans. Abbott also introduced enhanced safety labeling and full-spine imaging capabilities for patients implanted with Proclaim™ SCS systems and Penta™ paddle leads.
Expanded MRI access is critical, as nearly 84% of patients with spinal cord stimulators are expected to need an MRI within five years of implantation.
Advancing Personalized Neuromodulation for Chronic Pain
Abbott emphasized that its neuromodulation platforms are designed to evolve with patients over time, supporting long-term care needs through improved imaging compatibility and continued innovation. The company is investing in research focused on developing new stimulation waveforms, personalizing therapy, and leveraging data-rich systems to better understand how patients experience and communicate pain.
Ryan Lakin, Abbott’s vice president of neuromodulation, noted that chronic pain remains difficult to quantify, even in specialized clinical settings. Abbott aims to improve patient–physician communication and expand access to advanced therapies that help patients return to the lives they want to lead.
With new five-year evidence and expanded FDA-approved MRI capabilities, Abbott continues to strengthen its position in the neuromodulation field by delivering durable, patient-centered solutions for chronic pain management.
Understanding Neuromodulation
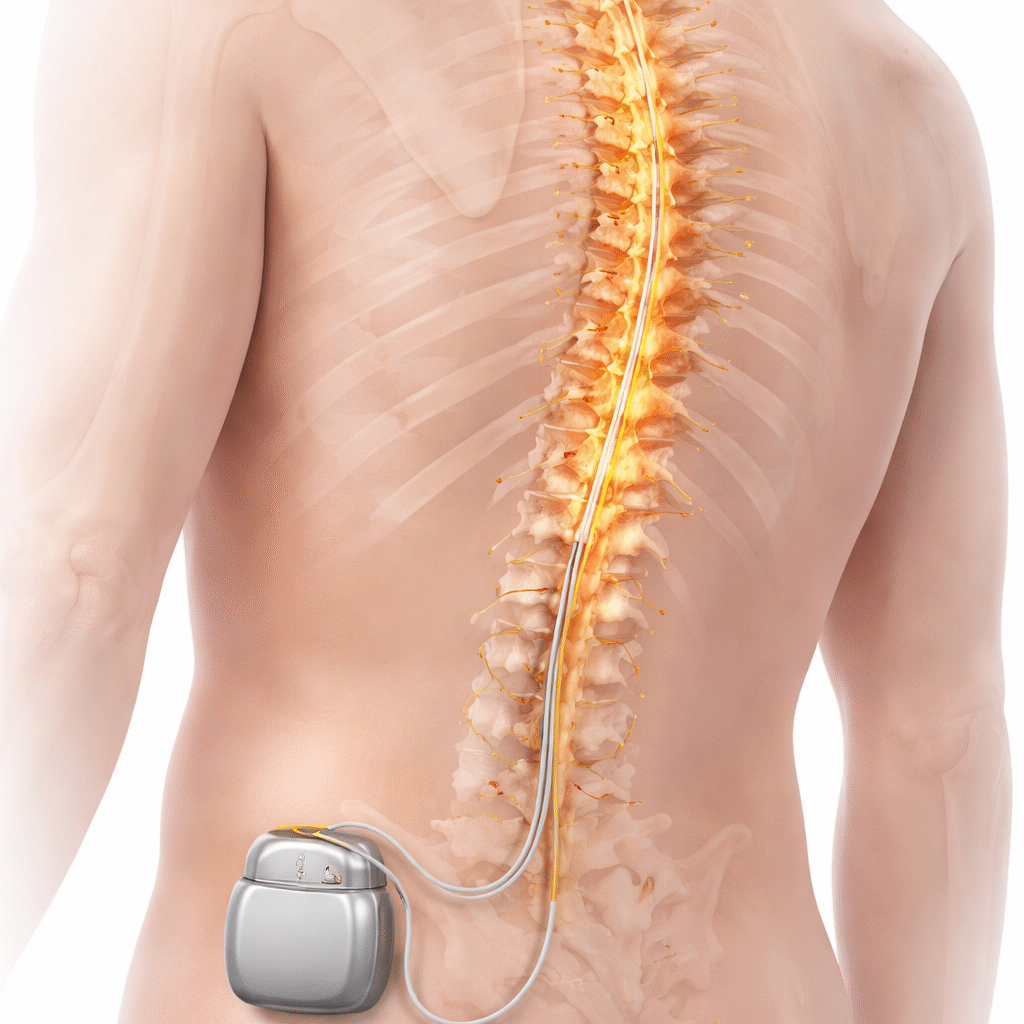
Abbott’s spinal cord stimulation (SCS) and dorsal root ganglion (DRG) stimulation therapies are implantable, drug-free neuromodulation devices designed to reduce chronic pain by delivering mild electrical pulses that modify pain signals before they reach the brain. Unlike medications, these systems do not rely on opioids or chemical treatment, but instead provide long-term pain control through advanced stimulation waveforms such as BurstDR™.
References
Five-year data shows Abbott neuromodulation systems reduce healthcare visits related to pain and deliver sustained relief, 23 January 2026, Abbott MediaRoom – Press Releases